 Imagine a man in his thirties—let’s call him Mike—comes into your practice. He is borderline obese and has diabetes. As a functional medicine professional, you determine that Mike has low testosterone, a vitamin D deficiency, and elevated homocysteine levels. Moreover, as a diabetic, he tells you he is taking a protein pump inhibitor and a diuretic.
Imagine a man in his thirties—let’s call him Mike—comes into your practice. He is borderline obese and has diabetes. As a functional medicine professional, you determine that Mike has low testosterone, a vitamin D deficiency, and elevated homocysteine levels. Moreover, as a diabetic, he tells you he is taking a protein pump inhibitor and a diuretic.
Now, given what you know, do you think Mike has a significant risk of osteoporosis later in life?
When you rely on incidents like broken bones to diagnose osteoporosis, you’re at a disadvantage from the start.
As it happens, each of our hypothetical patient’s attributes is in fact tied to developing osteoporosis in his later years. But our healthcare system often completely ignores these connections, leading to one of the major problems with osteoporosis: most people don’t know they have it until they start breaking bones.
Unfortunately, when you rely on incidents like broken bones to diagnose osteoporosis, you’re at a disadvantage from the start. Why? Fragility fractures are a lagging indicator, only alerting you to a problem after it’s materialized. It’s tough to get ahead of bone loss when you’re fighting from behind.
Bones Health Is Critical to Overall Health
And it’s not only fragility that you need to worry about when it comes to progressive bone loss. Far from being “just” the foundation upon which the body is constructed, bones support bodily health in a number of ways, including the following:
- Bones act as a reservoir for the body, storing essential minerals such as calcium, manganese, and vanadium.
- The body also funnels toxins to the bones to prevent them from being stored in our brain, organs, and tissues.
- Osteocytes (see below) play a role in blood sugar management, brain function, and the release of testosterone.
- Bone marrow is involved with hematopoiesis (the production of blood cells).
The body funnels toxins to the bones to prevent them from being stored in our brain, organs, and tissues.
The bottom line is that bone health is a critical component of overall health, which makes conditions like osteoporosis all the more important to understand, diagnose, and treat as early as possible.
However, in order to start spotting progressive bone loss earlier, we first need to understand the basics of bone remodeling.
What Is Bone Remodeling?
About 10 percent of skeletal mass is broken down and recreated each year in a process called bone remodeling. This is a cyclical process involving three specialized types of bone cells in the bone microenvironment: osteoclasts, osteoblasts, and osteocytes.
Osteoclasts originate in bone marrow and are responsible for removing damaged bone tissue. In effect, they “chew up” old bone that isn’t functioning well, resorbing bone material and dissolving the minerals contained within.
Bone remodeling is one of the body’s key functions for maintaining bone health.
Once the damaged bone material has been removed, osteoblasts come in and create new bone tissue, depositing new collagen and minerals. After rebuilding the bone, osteoblasts do one of three things:
- They flatten to the new bone, becoming protective bone-lining cells.
- They undergo apoptosis, or cell death, if no longer needed.
- They transform into osteocytes.
Osteocytes are the most common type of cell in mature bones. They are responsible for maintaining the bone matrix and act as sensors, signaling osteoclasts and osteoblasts to restart the remodeling process.
Bone remodeling is one of the body’s key functions for maintaining bone health. This process occurs throughout life, allowing the body to repair small flaws in bone, making bones thicker, and helping regulate mineral homeostasis.
When Bone Remodeling Goes Wrong
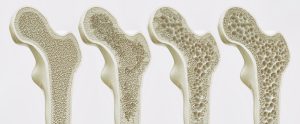
However, a key shift takes place with progressive bone loss conditions such as osteoporosis: osteoclast activity outweighs osteoblast activity. This causes greater rates of bone resorption and decreased rates of bone formation, leading to a net loss of bone volume and density, bone matrix disruption, and increased skeletal fragility.
Several factors can cause this unbalance. For one, chronic inflammation actually inhibits osteoblasts’ ability to create new bone. In fact, inflammation is one of the main contributors to bone loss. This means you could potentially prescribe a calcium supplement to a patient and see little to no change in bone loss—because calcium deficiency was never the underlying issue.
Body fat also promotes bone loss. Adipose tissue releases pro-inflammatory cytokines such as TNF-alpha, IL-6, and IL-1 into the body. These cytokines lead to increased osteoclast activity and inhibit osteoblasts, both of which directly impact bone remodeling. Not only that, but body mass index is correlated to inflammation, as well, making obesity a terrible one-two punch.
You could potentially prescribe a calcium supplement to a patient and see little to no change in bone loss—because calcium deficiency was never the underlying issue.
Additionally, hormone imbalances can lead to conditions like osteoporosis. Estrogen plays a role in both stimulating osteoblasts and inhibiting osteoclasts. Testosterone, by contrast, stimulates osteoclasts and inhibits osteoclasts, making a balance of these sex hormones crucial for bone remodeling. (Estrogens also play a very powerful role in managing inflammation responses.)
These are not the only factors to be aware of, but they do serve as a useful starting point. For more information about the causes of progressive bone loss, be sure to register for my Kharrazian Institute course, Degenerative Joint, Muscle, and Bone Conditions – Clinical Strategies and Treatment Applications. (See below for more information.)
Clinical Approaches to Bone Loss
Knowledge is powerful, but only when it is applied. So how can you successfully treat progressive bone loss in your patients?
Conventional medicine approach
In a pleasant turn of events, conventional medicine has begun to embrace what many might consider to be a true “functional medicine” solution: using vitamin D as a treatment for bone loss.
Vitamin D—which is really a hormone—helps maintain a crucial balance between osteoblasts and osteoclasts, which is essential for efficient bone remodeling. In fact, having chronically low vitamin D levels during your teens, 20s, and 30s is a significant red flag for being diagnosed with osteoporosis later in life.
Vitamin D helps maintain a crucial balance between osteoblasts and osteoclasts, which is essential for efficient bone remodeling.
Conventional medicine also makes use of a class of medications called bisphosphonates to mitigate bone loss. Bisphosphonates work by inhibiting the activity of osteoclasts, thus limiting the amount of bone they resorb. Of course, this does nothing to promote osteoblasts’ work, meaning they only truly address half of the bone-loss equation.
Functional medicine approach
The fact that bone-loss treatments such as vitamin D are seen as mainstream allows functional medicine practitioners to more easily work in concert with the conventional approach.
One way to come alongside the conventional approach is supplementation beyond vitamin D. Sodium is a phenomenal, yet overlooked, supplement that can be used to treat bone loss and bone density issues. Vitamin B helps reduce homocysteine (high levels of homocysteine promote bone resorption). Magnesium, turmeric, and resveratrol are also good options to consider.
When it comes to testosterone, hormone replacement therapy should be considered for patients over 40, especially if their muscle mass is low.
Taking steps to ensure hormonal balance is another key factor in treating your bone-loss patients. As mentioned above, testosterone and estrogen, along with thyroid hormones, all have powerful effects on bone health and remodeling. When it comes to testosterone specifically, hormone replacement therapy should be considered for patients over 40, especially if their muscle mass is low.
Focusing on movement is important as well. Physical movement helps build strong muscles, which in turn strengthen the bone(s) they are attached to. This is because osteocytes monitor mechanical stress in order to know when to signal remodeling—and much of that stress comes from our muscles.
And, of course, protocols for progressive bone loss should always include lifestyle changes to decrease bone-loss-causing inflammation. Developing good sleep habits, managing stress, and eating a healthy anti-inflammatory diet are all important contributors not just to bone health but overall wellness.
Degenerative Joint, Muscle, and Bone Conditions – Clinical Strategies and Treatment Applications by Dr. Datis Kharrazian
Progressive bone loss affects many millions of people worldwide, and especially the older population. Unfortunately, doctors tend to rely on cues like too-easily-broken bones to diagnose conditions such as osteoporosis because the current healthcare system tends to ignore other clear risk indicators.
Of course, the obvious truth is that the earlier we can spot bone-loss precursors in our patients, the more steps we can take to curb it before it spirals out of control. As the old saying goes, “an ounce of prevention is worth a pound of cure.”
The earlier we can spot bone-loss precursors in our patients, the more steps we can take to curb it before it spirals out of control.
Addressing conditions that could lead to osteoporosis early on, as opposed to waiting for lagging indicators, is one of the focal points of my new online course, Degenerative Joint, Muscle, and Bone Conditions – Clinical Strategies and Treatment Applications. In it, you’ll learn about the critical role of the musculoskeletal system’s metabolic functions and movement in chronic disease recovery.
I’ll also teach you how to identify and treat progressive bone loss conditions at their root to dramatically improve patient health outcomes. In addition, we’ll cover degenerative joint conditions, sarcopenia, muscle dysfunction, aging muscles, and principles and strategies to build muscle mass…and a lot more.
With this course, you’ll be empowered to address critical aspects of chronic disease management that often go overlooked and directly improve health outcomes for virtually every client you work with.
The course is open to licensed practitioners, medical doctors, nurse practitioners, health coaches, and other health professionals. You can register for this exciting course by clicking here.